Sensory Integration Therapy
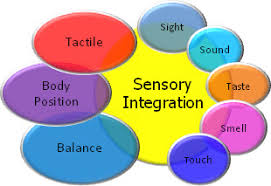
Sensory integration therapy was originally developed by occupational therapist A. Jean Ayres in the 1970s to help children with sensory-processing difficulties. It was specifically designed to treat Sensory Processing Disorder.
However sensory processing disorders are very common in autistic individuals. So here is a sample plan to help you get started if you are not able to book an appoint yet with an Occupational therapist. It is no alternative for a professional customized assessment and plan but it will equip you with the knowledge and strategies needed to support an individual with SPD.
Sensory Integration Plan
Purpose
This plan provides structured support for sensory processing needs, aiming to help the child regulate their sensory experiences and respond more adaptively to environmental stimuli.
Implementation should be done based on the individual’s :
- Specific sensory sensitivities
- Sensory-seeking behaviors
- Avoidance patterns
- Current coping strategies
- Environmental triggers
This plan covers all sensory domains except for olfactory and introspection. It can be used by parents, LSAs (learning support assistants), teachers and caregivers.
Sensory Domains and Interventions
1. Tactile (Touch) Integration
Calming Activities:
- Deep pressure activities
- Weighted blanket (check appropriate weight with OT)
- Bear hugs
- Compression vest (30 minutes on, 30 minutes off)
- Tactile exploration station
- Rice/bean bin
- Various texture swatches
- Therapeutic putty
Avoid:
- Unexpected light touch
- Crowded spaces
- Certain fabric textures (identify specific triggers)
2. Proprioceptive Input (Body Awareness)
Activities:
- Heavy work activities
- Carrying weighted backpack
- Wall pushes
- Animal walks
- Joint compression exercises
- Supervised jumping
- Climbing activities
- Resistance activities
- Therapy band exercises
- Push/pull games
3. Vestibular (Movement and Balance)
Structured Activities:
- Slow, rhythmic swinging
- Rocking chair
- Balance beam exercises
- Spinning (if tolerated, monitor responses)
Safety Measures:
- Always supervise movement activities
- Stop if signs of distress appear
- Allow breaks as needed
4. Auditory Processing
Environmental Modifications:
- Noise-canceling headphones
- White noise machine
- Quiet space designation
- Visual schedules for transitions
Calming Sounds:
- Nature sounds
- Preferred music
- Rhythmic beating
5. Visual Input
Environmental Adjustments:
- Reduce fluorescent lighting
- Use natural light when possible
- Minimize visual clutter
- Designated organized spaces
- Color-coding system for organization
6. Oral Motor/Oral Sensory
Activities:
- Chewy tubes
- Vibrating toothbrush
- Variety of food textures
- Drinking thick liquids through straws
Daily Schedule Integration
Morning Routine:
- Deep pressure exercises (10 minutes)
- Heavy work activity (5-10 minutes)
- Proprioceptive input before focused tasks
During Learning Activities:
- Movement breaks every 20-30 minutes
- Access to fidget tools
- Option to use alternative seating
- Visual schedule reference
Transition Periods:
- Warning signals (visual and verbal)
- Deep breathing exercises
- Movement activities between tasks
Calming Period/End of Day:
- Quiet space time
- Deep pressure activities
- Gentle swinging or rocking
Signs of Sensory Overload
Watch for:
- Covering ears or eyes
- Increased stimming
- Withdrawal
- Agitation
- Changes in breathing
- Verbal expressions of discomfort
Response Protocol:
- Remove from overwhelming environment
- Provide access to calming space
- Offer preferred sensory tools
- Use established calming routine
- Minimize verbal input
- Allow time to regulate
Progress Monitoring
Daily Documentation:
- Successful strategies
- Challenging situations
- New triggers identified
- Positive responses
- Areas needing adjustment
Weekly Review:
- Pattern identification
- Strategy effectiveness
- Environmental modifications needed
- Communication with team members
Team Coordination
Participants:
- Parents/Caregivers
- Occupational Therapist
- Teachers
- Support Staff
- Other Therapists
Communication Plan:
- Weekly progress updates
- Monthly team meetings
- Immediate notification of significant changes
- Shared documentation system
Emergency Response Plan
If Overwhelmed:
- Implement calming sequence
- Use designated safe space
- Contact primary support person
- Document incident
- Review and adjust plan as needed
Plan Review and Updates
- Formal review every 3 months
- Immediate updates as needed
- Parent/caregiver input regularly sought
- Professional consultation as required

Thanks I have recently been looking for info about this subject for a while and yours is the greatest I have discovered so far However what in regards to the bottom line Are you certain in regards to the supply
It’s hard to find knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks